3D PrintAbility
Everything clinicians need to scan, design, and print high-quality prosthetics and orthotics.
What Is 3D PrintAbility?
3D PrintAbility is an innovative toolchain we’ve developed alongside researchers at the University of Toronto.
It provides digital scanners, software called NiaFit, and 3D printers — everything a clinician needs to make a 3D printed prosthetic or orthotic.
3D PrintAbility improves on the traditional way of making prosthetics and orthotics by reducing the amount of time and money needed to make a device.
Meet 3D PrintAbility
A start-to-finish toolchain of digital scanners, custom software called NiaFit, and 3D printers — all of the tools clinicians need to scan, design, and print custom transtibial prosthetic sockets and AFOs for children and youth, aged 5-25.
Scan
The patient’s residual limb is scanned with a 3D digital scanner.
Design
A 3D model of the prosthetic socket or AFO is created using our software called NiaFit.
The device is printed on-site using a 3D printer. It is then assembled and fitted to the patient.
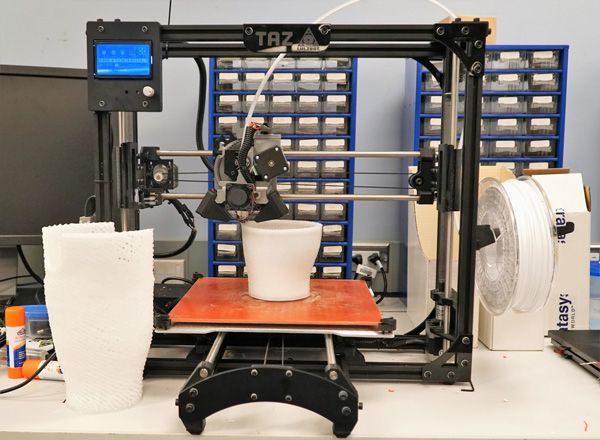
Watch A 3D Printer In Action
3D printing, or additive printing, is the process of producing a three dimensional object from a digital file using a special printer that lays downs material layer by layer.
Here’s a video of a 3D printer at work. The printer is producing a transtibial socket — a key component of a lower leg prosthetic.
Video: Time-lapse video of 3D printer making a prosthetic socket (0:22)
What Are The Benefits Of 3D PrintAbility?
How 3D Printing Compares With Handmade Methods
3D PrintAbility mirrors the manual fabrication process, but it does so in a digital environment. Here’s how the methods compare:
Traditional Method
- A plaster casting is applied by hand to the patient’s residual limb. Once the casting has dried, it’s used to create a mold.
- Any errors are fixed manually by adding or subtracting plaster to the mold.
- The mold is hand-wrapped in polypropylene to create the device. It is then cured in an oven.
3D PrintAbility Method
- A digital scanner is used by the clinician to create a 3D model of the patient’s residual limb.
- Any errors are flagged and fixed using our software called NiaFit.
- The digital model is sent to a 3D printer. The device is printed in about 6 hours and then assembled to fit the patient.
3D PrintAbility Is Safe And Effective
In 2017, we completed a large-scale clinical study of 3D PrintAbility at four sites across Cambodia, Tanzania, and Uganda. In total, approximately 140 children were fitted with 3D printed devices, including 70 transtibial prosthetics and 70 ankle-foot orthoses (AFOs). The results of the studies validated the durability, safety, and appropriateness of our devices.
We also tested the durability of our devices using a 1 million step robotic fatigue test — meeting the standards under ISO 10328:2006.
Alongside researchers at the University of Toronto, we continue to test, validate, and refine our technology to ensure we remain a global leader.